If you need to make a referral to the RMHS Case Management Agency, request an I/DD determination, apply for Medicaid, or obtain a PMIP, these RMHS guides can help. They walk you through each step of the process, making it easier to get the services and supports you need.
PLEASE NOTE:
Effective January 1, 2026: The Professional Medical Information Page (PMIP) must be submitted before an intake assessment can be held. You can view our guide to submitting the PMIP in English or Spanish.
Making a Referral to the CMA for Non-I/DD Clients
The three quick guides below will help you through the process of referring someone without an intellectual and developmental disability (I/DD) to the RMHS Case Management Agency. Select the guide that best matches your relationship to the person you are referring.
Referral Guide for Hospital, Nursing Facility, and PACE Staff
Use this guide if you are a staff member at a hospital, nursing facility, or PACE, and are making a referral for someone currently admitted in your facility.
Referral Guide for Other Providers
Use this guide if you work at an outpatient facility or provider agency and are making a referral for someone not currently admitted to a hospital or facility.
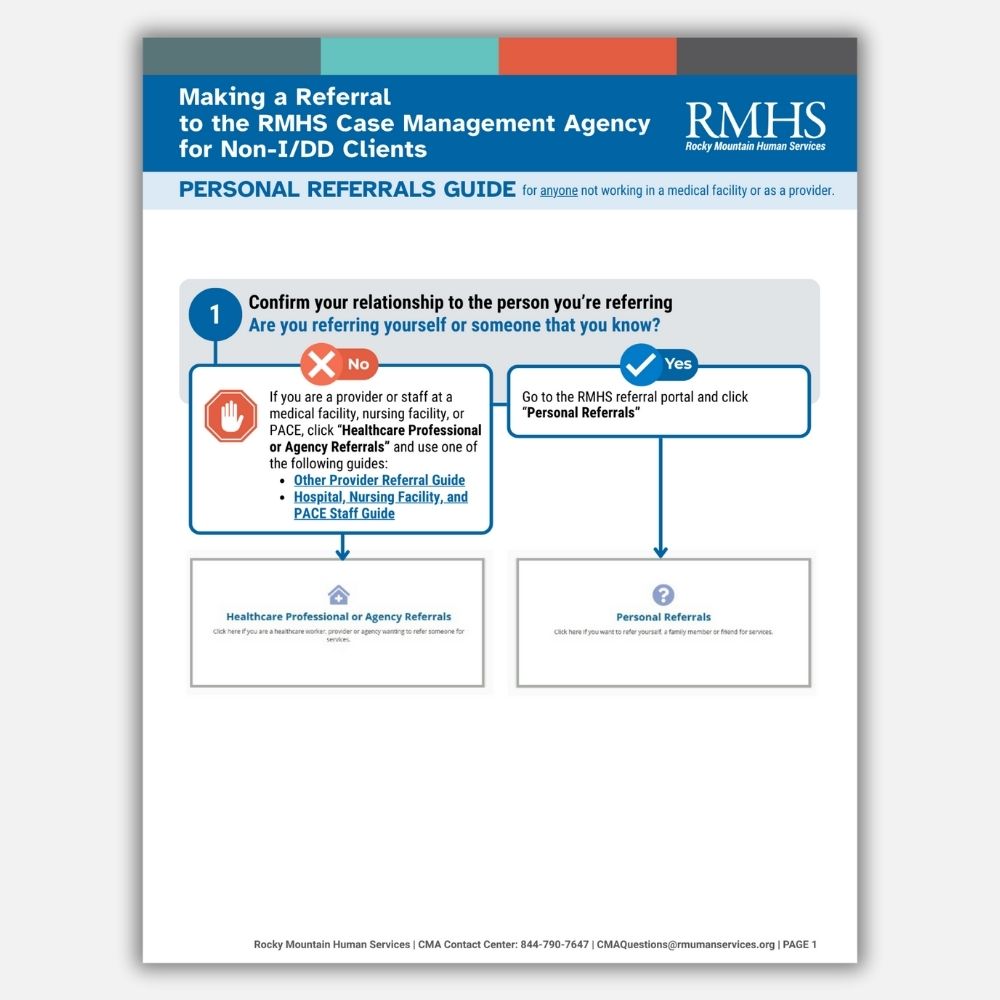
Personal Referral Guide
Use this guide if you are referring yourself or someone you know personally.
Enrolling in Services
The four quick guides below will help you through the process of enrolling in RMHS services, including filling out the Professional Medical Information Page (PMIP), applying for Medicaid financial eligibility, qualifying for Medicaid disability determination, and determining if you meet the developmental delay or I/DD criteria.
IMPORTANT NOTE: The Professional Medical Information Page (PMIP) must be submitted before an intake assessment can be held.
Completing the Professional Medical Information Page (PMIP) Form
This guide will walk you through the steps to fill out the PMIP form, which confirms that you or your child needs Long-Term Services and Supports.
Effective January 1, 2026: The Professional Medical Information Page (PMIP) must be submitted before an intake assessment can be held.
Applying for Medicaid Financial Eligibility
To access Long-Term Services and Supports, you must first qualify for Health First Colorado (Colorado’s Medicaid Program) by applying and meeting program-specific financial criteria. This guide will walk you through applying for Medicaid financial eligibility.
Applying for Medicaid Disability Determination
Colorado requires individuals to meet the disability criteria for Long-Term Services and Supports. This guide will walk you through applying for Medicaid disability determination.
Applying for a Developmental Delay or I/DD Determination
Certain Long-Term Services and Supports are designed for individuals with developmental delays or intellectual and developmental disabilities (I/DD). This guide will walk you through the process to determine if you meet the developmental delay or I/DD criteria to access those Long-Term Services and Supports.
Submit a Referral
Individuals, family members, and providers can all submit referrals. Please click Submit Referral to use our online portal and begin the process.
Contact RMHS Case Management Services
If you are not sure that you qualify for services, have trouble submitting a referral, or have questions, we have knowledgeable staff available to help.
CMA Contact Center: 844-790-7647
Email: CMAQuestions@rmhumanservices.org
If you are a provider interested in contracting with RMHS or looking for additional information, please visit our provider webpage here.
If you have a concern that you have been unable to resolve with your case manager, you can initiate an Escalation to help ensure you get the support and resolution you need or file a Case Management Agency Complaint Form.
RMHS Escalation Support Process
RMHS Case Management Agency Complaint Form






